Healthcare Professionals
Innovating non-invasive health monitoring with Bio Impedance
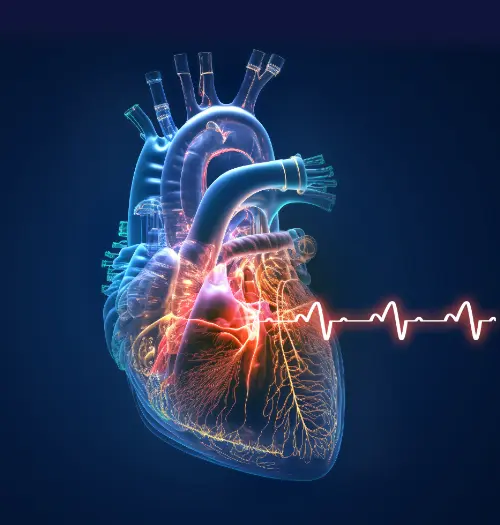
Impedance technology is based on Ohm's Law. Impedance (Zo) is the resistance to the flow of electrical current and is measured in ohms. Blood and other fluids are excellent conductors of electricity and have low impedance, particularly compared to bone, tissue, and air. Blood and fluid in the lungs are the most conductive substances in the thorax. Thus, larger quantities of thoracic fluid/blood lowers impedance and smaller quantities result in increased impedance.
Zo predominantly reflects total thoracic fluid volume, which is the overall thoracic resistance to flow of electrical current, reflecting thoracic fluid. The change in impedance is measured from the baseline impedance (Zo). The change in Z during systole is due to movement of blood and measures stroke volume. This change in impedance related to time (dZ/dt) generates a waveform that is similar to the aortic flow curve. Simultaneous recording of the ECG creates a timing-window for evaluation of each cardiac cycle. This measurement occurs between the opening and closing of the aortic valve. Our precise timing of this event and the ability to do this beat-to-beat quality measurement is why our device is more accurate than similar devices.